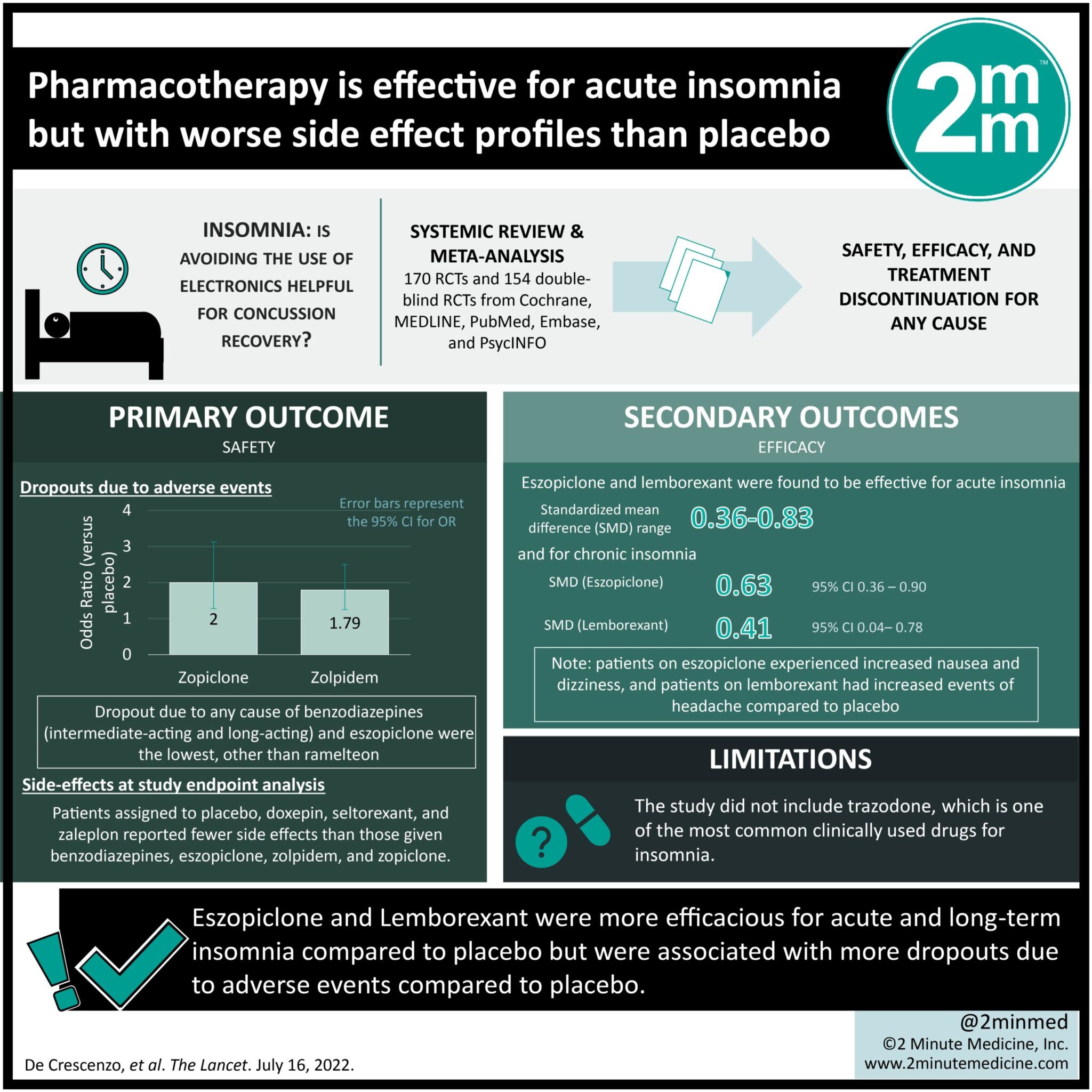
1. Eszopiclone and Lemborexant were more efficacious for acute and long-term insomnia compared to placebo but were associated with more dropouts due to adverse events compared to placebo.
2. Intermediate-acting benzodiazepines showed more acceptable tolerability compared to short-acting and long-acting benzodiazepines.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Insomnia is a common sleep disorder affecting 12-20% of adults worldwide. Although first-line therapy for insomnia includes conservative management, studies show that pharmacological measures may help improve insomnia. However, little is known about the comparative efficacies of the different pharmacological options available. This systematic review and meta-analysis aimed to study the safety and efficacy of pharmacotherapy for acute and chronic management of insomnia in adults. Primary outcomes included safety (≥1 adverse event), efficacy (patient-reported sleep quality), and treatment discontinuation due to any cause, while key secondary outcomes were sleep onset latency period, total sleep time, and number of awakenings. According to study results, pharmacological treatment of insomnia was associated with greater efficacy but more side effects than placebo, both in acute and long-term insomnia. In particular, eszopiclone and lemborexant were found to be more effective for both acute and long-term insomnia treatment compared to placebo and other pharmacologic interventions. Melatonergic drugs did not show a clear benefit over placebo. A limitation of this study is that it did not include trazodone which is one of the most common clinically used drugs for insomnia.
Click to read the study in The Lancet
Relevant Reading: Effect of Digital Cognitive Behavioral Therapy for Insomnia on Health, Psychological Well-being, and Sleep-Related Quality of Life: A Randomized Clinical Trial
In-depth [systematic review and meta-analysis]: This systematic review and meta-analysis included RCTs from Cochrane, MEDLINE, PubMed, Embase, and PsycINFO. Included were studies that used pharmacotherapy as first-line treatment for insomnia in patients ≥ 18 years, from start of databases to Nov 25, 2021. Altogether, 170 RCTs and 154 double-blind RCTs were included in the final systematic review and meta-analysis, respectively. With regard to the primary outcome of safety, more dropouts due to adverse events were reported in the zopiclone (odds ratio [OR] 2.00, 95% confidence interval [CI] 1.28-3.13) and zolpidem (OR 1.79, 95% CI 1.25-2.50) groups versus placebo. Furthermore, patients assigned to placebo, doxepin, seltorexant, and zaleplon reported fewer side effects than those given benzodiazepines, eszopiclone, zolpidem, and zopiclone. Eszopiclone and lemborexant were found to be effective for acute insomnia (standardized mean difference [SMD] range 0.36-0.83) as well as chronic insomnia (eszopiclone: SMD 0.63 [0.36-0.90]; lemborexant: SMD 0.41 [0.04-0.78]) compared to placebo. However, eszopiclone was associated with increased nausea and dizziness while lemborexant had increased events of headache compared to placebo. Eszopiclone (OR 0.43, 95% CI 0.20-0.93) and zolpidem (OR 0.43, 95% CI 0.19-0.95) also had a lower rate of all-cause discontinuation than ramelteon; for zolpidem, the rate was higher than placebo (OR 2.00, 95% CI 1.11-3.70). Overall, findings from this study suggest that although pharmacological treatment may benefit in the short-term, long-term safety and efficacy remains unclear.
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.