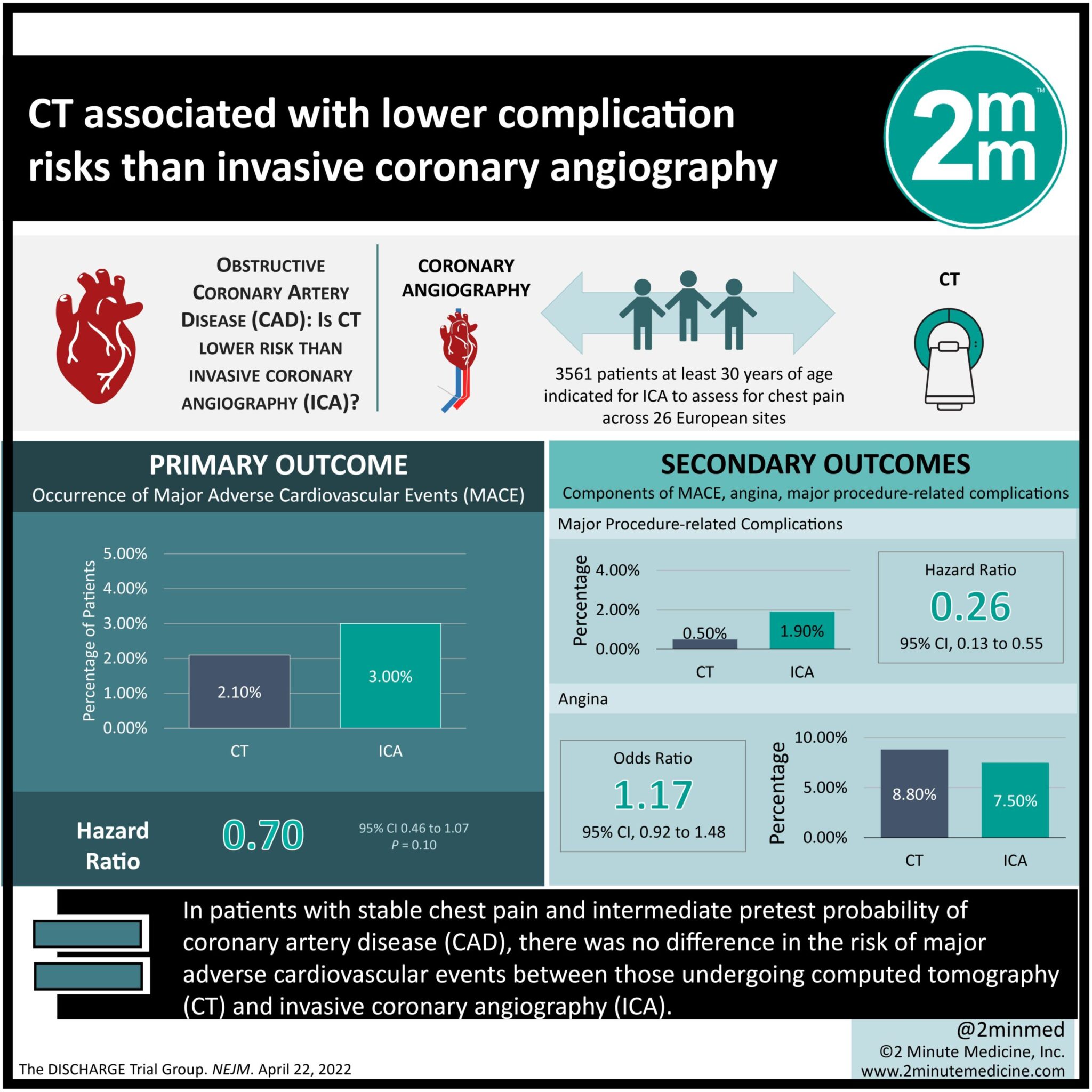
1. In patients with stable chest pain and intermediate pretest probability of coronary artery disease (CAD), there was no difference in the risk of major adverse cardiovascular events between those undergoing computed tomography (CT) and invasive coronary angiography (ICA).
2. CT was associated with fewer procedure-related complications than ICA.
Evidence Rating Level: 1 (Excellent)
Study Rundown: In patients with stable chest pain and intermediate pretest probability of obstructive CAD, ICA is the reference standard of diagnosis and allows for revascularization therapy should an obstruction is found. Nevertheless, elective ICA in such a patient population is associated with rare but major procedure-related complications, while only potentially detecting obstructions in 50% of the patients undergoing this procedure. CT is an accurate, non-invasive alternative to ICA that can rule out obstructive CAD and identify revascularization therapy candidates with lower risks of ICA-related complications. The current study compared CT against ICA as an initial diagnostic step for patients with stable chest pain who were referred for testing. Over 3.5 years, patients undergoing CT were found to be at similar risk of developing major adverse cardiovascular events (MACE) and angina, when compared to the ICA group. However, procedure-related complications occurred less frequently among patients in the CT group. Overall, these results add to the body of evidence supporting the use of CT as the first diagnostic step over ICA, to guide the management of patients with stable chest pain.
Click here to read the study in NEJM
Relevant Reading: Evaluation of computed tomography in patients with atypical angina or chest pain clinically referred for invasive coronary angiography: randomised controlled trial
In-Depth [randomized controlled trial]: The current study was a multicenter, pragmatic, randomized trial comparing CT against ICA as an initial diagnostic test to guide the management of patients with stable chest pain and an intermediate pretest probability of CAD who had been referred for ICA. 3561 patients (56.2% were women) were enrolled and analyzed across 26 European sites. Eligible patients were at least 30 years of age and clinically indicated for ICA to assess their chest pain. Intermediate pretest probability was defined as between 10 and 60% based on a validated calculator. Patients were excluded if they received hemodialysis, lacked sinus rhythm, or were pregnant. Patients were randomized 1:1 to undergo CT or ICA. Patients were discharged if obstructive CAD was ruled out, whereas positive CAD findings prompted guideline-recommended treatment, including medical and revascularization therapies. The primary outcome was the occurrence of MACE, a composite measure of cardiovascular death, nonfatal myocardial infarction, and stroke. Secondary outcomes included the components of MACE, angina, and major procedure-related complications. Outcome assessors were blinded to the group assignments. The median follow-up was 3.5 years and outcomes were assessed through a modified intention-to-treat analysis. The composite MACE occurrence was 38 of 1808 patients (2.1%) in the CT group and 52 of 1753 patients (3.0%) in the ICA group (hazard ratio [HR], 0.7; 95% confidence interval [CI], 0.46 to 1.07; P=0.10). The rates of each component MACE were comparable between both groups. Major procedure-related complications (from the diagnostic ICA and indicated revascularization procedures) occurred in 9 patients (0.5%) of the CT group and 33 patients (1.9%) of the ICA group (HR, 0.26; 95% CI, 0.13 to 0.55). The expanded composite outcome of MACE and procedure-related complications occurred in 50 patients (2.8%) of the CT group and in 80 patients (4.6%) of the ICA group (HR, 0.60; 95% CI, 0.42 to 0.85). The incidence of angina was 8.8% in the CT group and 7.5% in the ICA group (odds ratio, 1.17; 95% CI, 0.92 to 1.48). The study limitations included unblinded group assignments and a potential bias favoring the ICA group. Notwithstanding, its pragmatic design, high protocol adherence, and complete follow-up bolstered its results. Overall, the study showed that, compared to ICA, utilizing CT as an initial test was associated with similar MACE outcomes but a lower risk of procedure-related complications for patients with stable chest pain.
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.