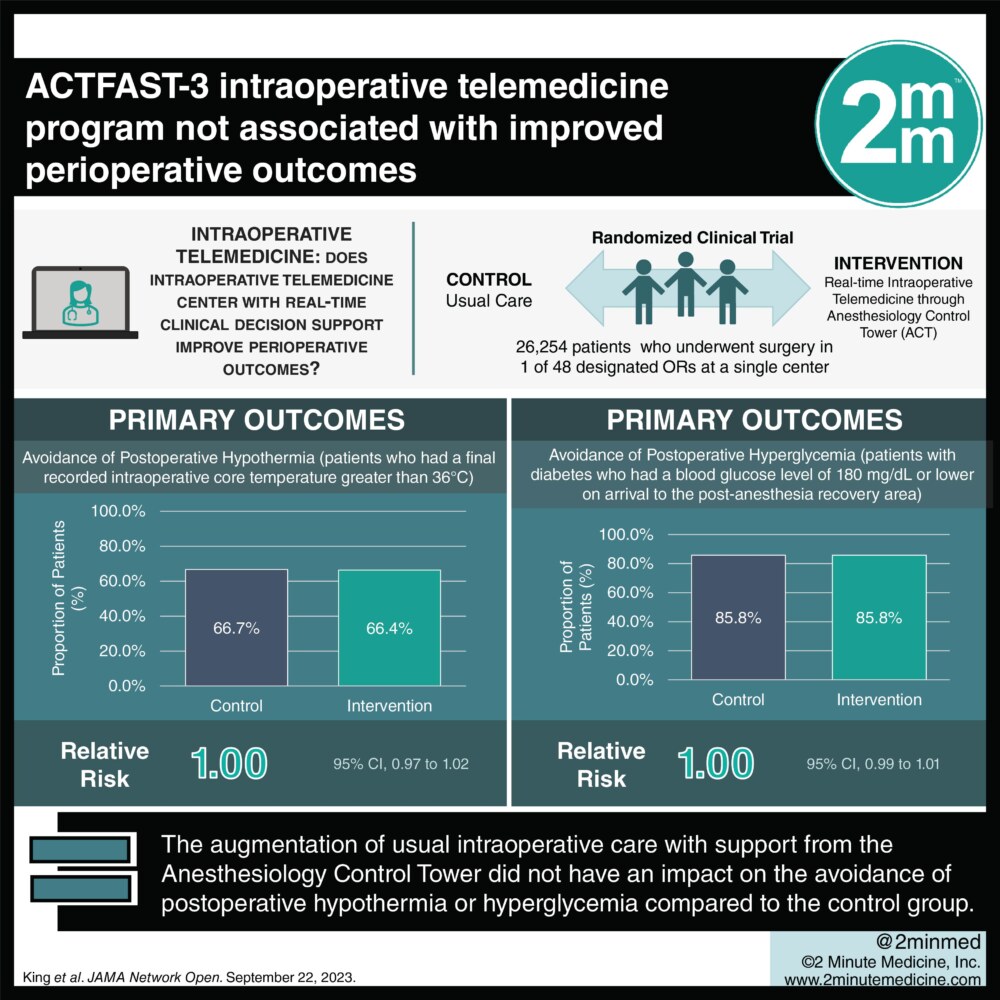
1. The augmentation of usual intraoperative care with support from the Anesthesiology Control Tower (ACT) did not have an impact on the avoidance of postoperative hypothermia or hyperglycemia compared to the control group.
2. While there was no significant difference in other secondary or clinical outcomes, appropriate intraoperative glucose measurement was more common among patients with diabetes in the intervention group.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Telemedicine—defined by the World Health Organization as using communication technologies for diagnosis and treatment—has seen significant growth over the past decade. In anesthesia, it has been applied in preoperative assessments, remote intraoperative monitoring, and postoperative care. Clinical decision support tools have been found to improve some quality outcomes, but the burden of alert fatigue reduces the benefit of decision support. Filtering of decision support alerts by telemedicine clinicians may mitigate alert fatigue and reduce oversights in care. The ACT combines remote intraoperative monitoring with customized clinical decision support. The Anesthesiology Control Tower–Feedback Alerts to Supplement Treatments (ACTFAST-3) is a single-center pilot superiority randomized clinical trial that aims to evaluate the impact of ACT on two quality of care measures: postoperative hypothermia and hyperglycemia. Patients aged 18 years or older who underwent surgery in designated ORs at the study site, Barnes-Jewish Hospital and Washington University School of Medicine, from April 2017 to June 30 were included in the analysis. Designated ORs, were randomized to the control group, usual intraoperative care, and the intervention group, usual intraoperative care with telemedicine decision support from the ACT intraoperative care. For primary outcomes, there was no significant difference in the avoidance of postoperative hypothermia or postoperative hyperglycemia between the intervention and control groups. Aside from a significant increase in the incidence of appropriate intraoperative glucose measurements, there was no significant difference in any secondary outcomes (hypotension, temperature monitoring, timely antibiotic redosing, neuromuscular blockade monitoring, ventilator management, and volatile anesthetic overuse) or clinical outcomes. Overall, these findings demonstrated that support from an intraoperative telemedicine center with real-time clinical decision support did not affect intraoperative quality of care measures. However, This RCT established a model for real-time intraoperative telemedicine and suggests improved outcomes may be achieved by streamlining clinical decision support and workflows.
Click to read the study on JAMA Network Open
In-Depth [randomized controlled trial]: The ACT involves ACT clinicians overseeing multiple ORs and filtering decision support alerts to offer preemptive recommendations to intraoperative anesthesiologists. The ACTFAST-3 randomized clinical trial aims to evaluate the efficacy of ACT on the avoidance of postoperative hypothermia, patients who had a final recorded intraoperative core temperature greater than 36°C, and avoidance of postoperative hyperglycemia, patients with diabetes who had a blood glucose level of 180 mg/dL or lower on arrival to the postanesthesia recovery area. A total of 26,254 adults who underwent surgery in 1 of 48 designated ORs, were included in the analysis. Designated ORs (rather than patients) were randomized in a 1:1 ratio to the control or intervention groups, with patients and clinicians (unless they were contacted by ACT) remaining blinded. 13,274 patients (mean age [IQR] 59 [47-69] years, 51.5% female) comprised the control group that received usual intraoperative care, while 12 980 patients (mean age [IQR] 60 [47-69] years, 50.5% female) comprised the intervention group, receiving usual care augmented with telemedicine decision support from the ACT. There was no significant difference in the avoidance of hypothermia (66.4% in the intervention group vs. 66.7% in the control group RR, 1.00; 95% CI, 0.97-1.02) or postoperative hyperglycemia (85.8% in the intervention group vs 85.8% in the control group; RR, 1.00; 95% CI, 0.99-1.01) between groups. However, the intervention group demonstrated a significant increase in the incidence of appropriate intraoperative glucose measurement among patients with diabetes (RR, 1.07; 95% CI, 1.01-1.15; Holm-corrected P = .02). There was no significant difference in other secondary outcomes (intraoperative hypotension, temperature monitoring, timely antibiotic redosing, neuromuscular blockade monitoring, ventilator management, and volatile anesthetic overuse) or clinical outcomes (30-day mortality, 30-day readmission, and postoperative acute kidney injury).
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.