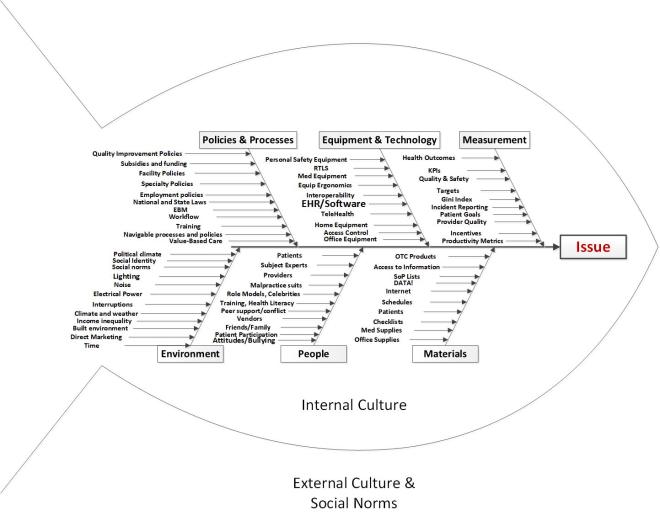
On October 25, 2018, Physician’s Weekly co-hosted a live, interactive tweetchat on ICU safety with Kelly Cawcutt, MD, and MEQAPI (Monitoring & Evaluation, Quality Assurance, and Process Improvement). Topics to be discussed take the #MEQAPI tweetchat “fishbone” approach:
Topics discussed hit the six main areas in the fishbone: Policy: What laws, policies, rules, regulations, etc. enhance or degrade safety in the ICU. Equipment: How equipment and devices enhance or degrade safety in the ICU. Measurement: How quality, safety, and performance metrics enhance or degrade safety. Environment: What environmental factors cause your issue, what are potential solutions to your issue? People: How do the people in healthcare – the staff, cleaners, technicians, clinicians, researchers, public, media, friends, family, etc cause your issue, what are potential solutions to your issue? Materials: What “medical stuff” that patients need cause your issue, what are potential solutions to your issue.
Below are the highlights from the chat. You can read the full transcript here, by scrolling down to the corresponding responses.
Click here for a look at our #PWChat schedule and recaps.
Question 1
T1: Policy: What laws, policies, rules, regulations, etc. enhance or degrade safety in the #ICU?
— Physician’s Weekly (@physicianswkly) October 26, 2018
A1. This reply is through my lens of Program Director, but I believe duty hour restrictions for trainees are useful thing in an ICU setting, given the intense environment and fatiguability. However, the more frequent the transitions of care, the more room for error. #PWChat
— Amy Oxentenko M.D. (@AmyOxentenkoMD) October 26, 2018
That last part is a really good point; is that from poor communication or things being forgotten when, for example, day shift nurse handoffs to night shift nurse?#PWChat
— Physician’s Weekly (@physicianswkly) October 26, 2018
RN to RN, RT to RT, MD to MD. There are A LOT of handoffs in the ICU.
— Kelly Cawcutt MD MS (@KellyCawcuttMD) October 26, 2018
Checklist policies in the icu can enhance safety especially when team members are empowered to speak up. When nurses point out that the catheter has been in for 3 days and the pt is ambulatory so time to get it out, ICU policies to support that help get the job done #PWChat
— Jasmine R Marcelin, MD (@DrJRMarcelin) October 26, 2018
Question 2
#PWChat
T2: Equipment: How do equipment and devices enhance or degrade safety in the #ICU?— Physician’s Weekly (@physicianswkly) October 26, 2018
From an infectious diseases standpoint, when I see the various lines and catheters all I see are potential hospital acquired infections! Acknowledging that we need these to keep people alive in the ICU, still important to reassess necessity daily and get them out! #PWChat
— Jasmine R Marcelin, MD (@DrJRMarcelin) October 26, 2018
A2. Equipment/devices bring the benefit of added technology to diagnose and manage disease, but bring the issues of infection control, device malfunction, and overreliance on devices rather than using clinical judgement/acumen. #PWChat
— Amy Oxentenko M.D. (@AmyOxentenkoMD) October 26, 2018
With regards to Dr. Oxentenko’s point, devices may give us information, but it is up to the clinician to interpret correctly. For example, studies have shown variable results in correct interpretation of PA catheter numbers. So devices can enhance and degrade care. #PWChat
— Emily Methangkool MD, MPH (@dremilym) October 26, 2018
Question 3
#PWChat
T3: Measurement: How do quality, safety, and performance metrics enhance or degrade safety in the #ICU?— Physician’s Weekly (@physicianswkly) October 26, 2018
I think metrics are useful when we know a benchmark or comparison. Knowing where you are in comparison to others makes driving for improvement more meaningful. When people are motivated to improve quality, safety will improve too. #PWChat
— Jasmine R Marcelin, MD (@DrJRMarcelin) October 26, 2018
Question 4
T4: Environment: What environmental factors enhance or degrade safety in the #ICU? Everything from the room where care is provided, facility location, privacy, etc.
— Physician’s Weekly (@physicianswkly) October 26, 2018
Close proximity to procedural locations is important for ICU patients. The last time a critically ill patient spends in transit the better. It would be nice to have the OR or IR suite on the same floor as the ICU. #PWChat
— Emily Methangkool MD, MPH (@dremilym) October 26, 2018
Also goes similar to previous discussions about sleep, but having call rooms near the icu? Potentially could make a world of difference in a 24hr shift if u could rest nearby but be close enough to respond if needed. If call rooms far, maybe u won’t rest & without rest… #PWChat
— Jasmine R Marcelin, MD (@DrJRMarcelin) October 26, 2018