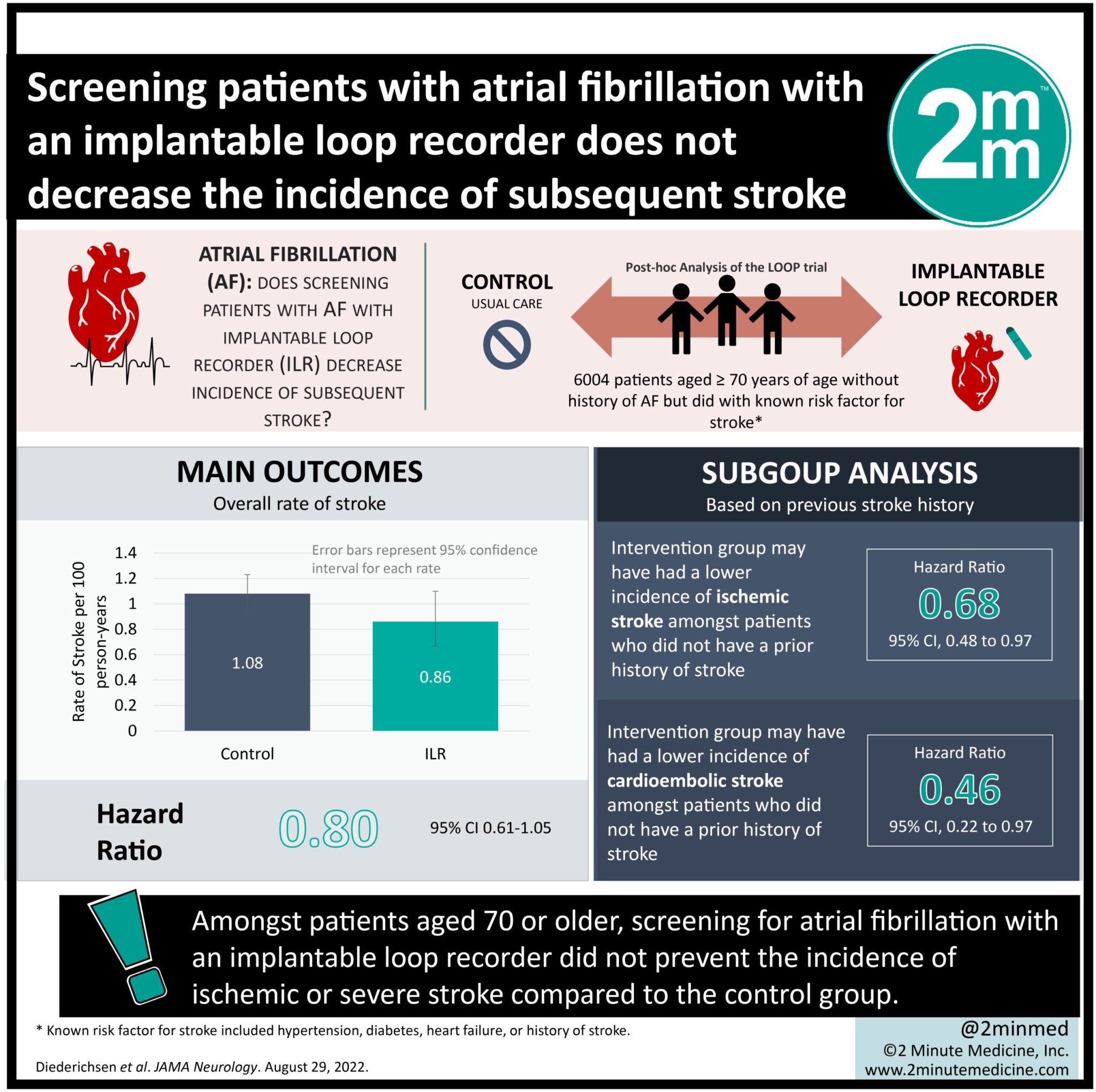
1. Amongst patients aged 70 or older, screening for atrial fibrillation with an implantable loop recorder did not prevent the incidence of ischemic or severe stroke compared to the control group.
2. Subgroup analysis revealed that implantable loop recorders may reduce stroke incidence in patients who had not previously had a stroke.
Level of Evidence Rating: 1 (Excellent)
Study Rundown: Atrial fibrillation is an important risk factor for stroke which is often underdiagnosed and poorly controlled. Means of extended cardiac monitoring with a device such as an implantable loop recorder (ILR) can improve the ability to detect when a patient is experiencing atrial fibrillation. In theory, this may also indicate times at which their risk of embolic event (i.e., stroke or transient ischemic attack) is increased. The present randomized controlled trial sought to determine whether ILR can prevent stroke in patients aged 70 or older who have at least one other risk factor for stroke.
6004 patients were followed in this study, including 4503 in the usual care (control) group and 1501 in the ILR group. Baseline characteristics were balanced between the two groups. 1027 patients were diagnosed with atrial fibrillation during the study period including 550 (12%) in the ILR group and 477 (32%) in the control group. 5.2% of patients in the study had a stroke during the study period including 5.5% of patients in the control group and 4.4% of patients in the ILR group. The overall rate of stroke was not significantly different between patients in the control and the ILR groups. 2.0% of patients had a severe stroke according to standard classification; this was not significantly different between the control and experimental groups.
This randomized controlled trial demonstrated that there is no overall difference in stroke rate amongst patients aged 70 or older at risk for stroke whether they have an ILR in place or not. Although, there may be some benefit in patients with no history of prior stroke. Further research should work to develop effective interventions for this group of patients when they are identified to be at higher risk of stroke to improve outcomes. A strength of this work includes the randomized design which does well to control for confounding variables. However, this study is limited as data was analyzed retrospectively, being a post hoc analysis.
Click here to read this study in JAMA Neurology
Relevant reading: Atrial fibrillation and mechanisms of stroke: time for a new model
In Depth [randomized controlled trial]: This article reports the post-hoc analysis of the LOOP trial which was conducted at several centers in Denmark as a randomized controlled trial. Individuals aged 70 or older who had no history of atrial fibrillation but did have a known risk factor for stroke (i.e., hypertension, diabetes, heart failure, history of stroke) were included; a baseline electrocardiogram was then used to exclude patients with atrial fibrillation. Patients were randomized (1:3) to receive either ILR with remote monitoring or usual care. Patients were followed with in-person study visits for at least 3 years, with a median follow up period of 65 months (interquartile range 59-70 months). Stroke diagnoses were assessed by a group of expert clinicians and subsequently grouped based on the length of stay in hospital and severity at presentation.
The overall rate of stroke in the control group was 1.08 per 100 person years (95% confidence interval 0.95-1.23) and was 0.86 (0.67-1.10) per 100 person years in the ILR group. The hazard ratio for stroke in the ILR group compared to the control group was 0.80 (0.61-1.05), which was not significantly different. The proportion of severe stroke was 40% in the control group and 35% in the intervention group. The hazard ratio for severe stroke between groups was 0.69 (95% confidence interval 0.44-1.09). A subgroup analysis based on previous stroke history found that the intervention group may have had a lower incidence of ischemic stroke amongst patients who did not have a prior history of stroke: hazard ratio 0.68 (0.48-0.97). The same was true for cardioembolic stroke, as evidenced by a hazard ratio of 0.46 (0.22-0.97).
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.